The FDA outlines draft guidance on AI for medical devices
The agency also published draft guidance on the use of AI in drug development
Read more...Aexa watched in horror as her 65-year-old husband slipped off the sock from his right foot  one night before bed, two weeks into the COVID-19 Shelter-In-Place mandate. A pea-sized sore on Jack’s foot just weeks before had exponentially grown to cover one-quarter of his foot, where several toes had been amputated prior.
one night before bed, two weeks into the COVID-19 Shelter-In-Place mandate. A pea-sized sore on Jack’s foot just weeks before had exponentially grown to cover one-quarter of his foot, where several toes had been amputated prior.
She asked, “Jack, does it hurt?”
“Yes, I haven’t slept more than a couple of hours a night for a week,” he responded.
First thing the next morning Jack called his Vascular Surgeon at a large well-known big city Hospital. Jack’s Vascular Surgeon told him he would need blood flow restored within days to save his foot. He said the bad news was that restoration was not possible because COVID-19 had overwhelmed the Hospital and no surgery rooms would be available for weeks. By then, he said, it would be too late — the foot would be too far gone to save. So, the best he could do would be to schedule an amputation for one month from that date.
Alexa heard about “The Way To My Heart,” a 501c3 nonprofit, which I started a year ago to help patients avoid needless amputations due to Peripheral Artery Disease (PAD), a disease denoted by blocked arteries mainly in the legs, that impacts 1 in 20 people over age 50, and 1 in 3 Diabetics over age 50. She reached out to vent and get support from our wellness team for her husband to wrap his mind around life beyond amputation. Instead, we connected her to an Office-Based Lab (OBL) where the Interventional Cardiologist was specifically trained in cutting-edge, below-the-knee revascularization.
Alexa and her husband packed up their car and drove three hours to see this Doctor who saved Jack’s leg from amputation. Six weeks later, his foot ulcers are healing and he is walking one mile per day pain-free, whereas before the procedure he could barely limp to the bathroom without debilitating foot and leg pain.
Alexa and Jack are not alone during this pandemic. Their story is similar to many others we help through The Way To My Heart who were told by Hospital Doctors to delay procedures that would restore blood flow to help their diabetic foot ulcers heal and prevent amputation. U.S. Hospital Surgeons already perform more than 200,000 needless amputations a year due to Peripheral Artery Disease for two reasons:
The number of amputations is likely to be higher this year due to the pandemic and recommendations to shelter in place and quarantine which is causing more people over the age of 50 to be sedentary.
While a sedentary lifestyle increases the potential for plaque to build-up in arteries, patients are not seeking treatment before diabetic ulcers appear and ultimately turn gangrenous. When patients do seek treatment in a Hospital they’re being turned away, and many do not know about limb-saving options such as what Alexa and Jack discovered. So, by the time they can get in to see the Hospital Doctor, the infection is too deep, and amputation is the only option.
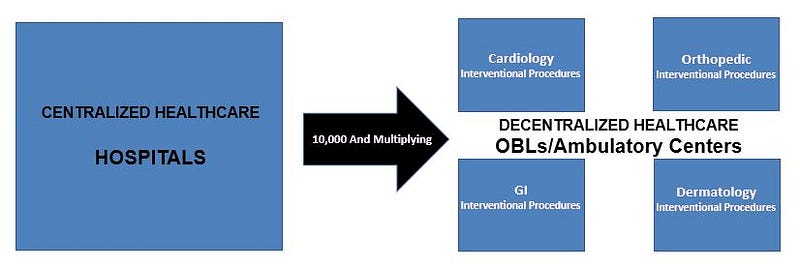
COVID-19 has highlighted the critical need for Office-Based Labs (OBL) and Ambulatory Surgical Centers (ASC), especially for patients with Peripheral Artery Disease and other comorbidities that can lead to deadly complications from viruses such as COVID-19 and Influenza. OBLs are focused solely on limb salvage and patient care is less likely to be disrupted. OBLs are also a safer place to treat these patients due to a regular, moderately sized staff and patients who only make appointments for vascular-related illness. Even if a Hospital Doctor could perform a limb salvage procedure during this pandemic, these PAD patients would be at greater risk of contracting COVID-19 while being treated inside the same building and by sometimes the same staff as patients with contagious viruses.
OBLs offer significant advantages for patients in need of revascularization:
Considering all the aforementioned advantages of OBLs, patients especially with comorbidities such as PAD, should strongly consider this fast-growing option to ensure quick, timely, and safer treatment for a better quality of life. Hospitals are starting to recognize the value of OBL’s as well. Some are expanding their affiliations to include them under their umbrella. It is a smart move on their part. A decentralized model best serves these patients and its been proven safe, even in rural communities.
The largest study of its kind conducted in a rural community with nearly 700 PAD patients recently concluded that "Endovascular procedures for PAD can be performed safely in a rural outpatient setting with low complication rates." That's important because a decentralized model alone does not solve the problem of access to minimally invasive treatment options for the most at-risk communities. The Author of the study, California Heart & Vascular Clinic's Dr. Athar Ansari futher concluded that, "Outpatient procedures for PAD are safe and may widen access to specialist procedures in areas of socio-economic deprivation."
The key is to open more OBLs in areas most at risk for amputation, particularly in the South, where African Americans are three times more likely than their white counterparts to have a limb amputated due to PAD. Multiple factors contribute to that including fewer available specialists in these areas, lack of education about treatment options outside of hospitals, lack of insurance to provide access to early diagnosis and treatment, as well as blatant discrimination.
A major catalyst that drove me to start The Way To My Heart was a confrontation with a Vascular Specialist in the South, whom I was observing for the day, who told a black man that amputation was his only option. After the man left, I shared with the physician that I was surprised in his treatment option after observing his success using minimally invasive techniques to unblock arteries in what seemed to be more complex cases earlier in the day. His response still haunts me today. He said…
“This would be my third time unblocking his arteries and because he’s a black man
from the projects he just doesn’t take care of himself, eat right, exercise, and
he smokes so he’ll just be back again for yet another procedure so why delay the
inevitable as we will have to amputate at some point.”
I told this Doctor directly, point blank, “I’m disappointed. Here is my card. Don’t
amputate. Send this man to me and I’ll help him with food access and lifestyle
modification support including smoking cessation. He will NOT be back to see you.”
That doctor never sent me that patient, but since that day, through The Way To My Heart, which educates, engages, and empowers patients to take their healthcare into their own hands, I’ve helped hundreds of patients across America to find a physician who would exhaust efforts to save their legs from amputation, including Jack. We’ve also supported hundreds more through our “My Steps” program to take ‘microsteps’ to better health with real-time support for critical lifestyle modifications, which includes access to healthy food options thanks to RightRice and our partnership with VitaBowl.
Alexa and Jack are glad they discovered The Way To My Heart, and ultimately, through us, their OBL Vascular Specialist. Jack’s recovering now from having arteries in his left leg unblocked and hopes to reach his goal of walking two miles per day by the end of summer. He is working with our performance coach on a customized exercise program free -of-charge to help him reach his goals and prevent a revolving door of treatment.
The agency also published draft guidance on the use of AI in drug development
Read more...The biggest focus areas for AI investing are healthcare and biotech
Read more...It will complete and submit forms, and integrate with state benefit systems
Read more...