Perseverance: From running out of money to an IPO - StubHub comes back strong
In the post-Covid drive for live events, ticket platforms are jumping at the opportune market time
Read more...
When Haris and I started our startup journey a few years ago, we had both recently struggled with our Mental Health. I was recovering from a depressive burnout after overworking myself, and he was having panic attacks out of the blue. Both of us, decided to start psychotherapy, and quickly realized that psychotherapy -although extremely helpful, and probably the best investment we’ve done in our lives- was happening in an outdated way and needed to be modernized.
We also realized that we were not alone in this. Mental health disorders are on the rise. The numbers speak for themselves. According to the World Health Organization, close to half a billion people globally suffer for some sort of mental health illness. One in five people in the US today are dealing with an illness that impacts their mental state. To put it in context, this statistic outnumbers the entire population of California. Today depression is affecting 300 million people worldwide. What’s worse is that the National Institute of Mental Health estimates that by 2030, depression is expected to be the leading cause of disease burden globally.
While mental health disorders are on the rise, so is the demand for mental health care services. But, the current healthcare system can not keep up. Mental health disorders cost $467 billion annually to the US economy.
On top of that, behavioral health issues are a key predictor of high costs. Among the population suffering from chronic disease, those with a mental illness cost between to 2 and 3 times more than those without. Care providers have not yet adequately responded to the burden of mental health disorders while poor quality of care continues to be a problem for many patients who receive treatment. What are the culprits you might ask? Several reasons.
The current model for mental health care has seven major flaws:
AI, IoT and digital therapeutics enable a new era in Mental Health
Innovation in mental health is long overdue. While modern medicine relies almost solely on objective measurement, mental health has remained in the domain of subjective reporting. Its clinical environment hasn’t evolved with the intelligence, care, and diagnostics shown to the rest of medicine. To diagnose and track mental health issues we still rely on patient questionnaires.
In other medical and life sciences fields, practitioners and patients utilize a variety of tools and technologies. For example, cardiologists use blood pressure monitors to objectively evaluate and monitor situation of the patient. Diabetics regulate their intake of insulin and diet based on measurements taken from mobile glucose monitors. Telemedicine technologies have boomed in the healthcare sector, while mental health technology lagged behind.
BUT IT DOESN’T HAVE TO BE THAT WAY, because nowadays with the evolution of IoT, AI, mobile and digital health technologies we can have:
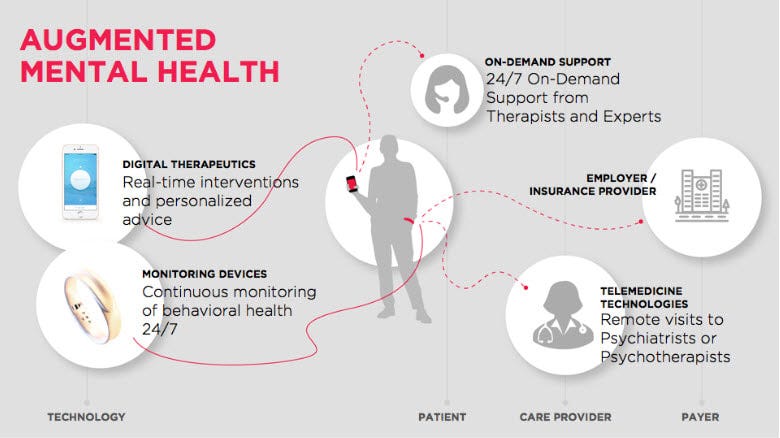
Enter the era of Augmented Mental Health
In the Augmented Mental Health era, patients receive personalized care and support around the clock, families are automatically notified when their loved ones are at risk and therapists base their diagnosis on objective data.
Similar to how diabetics use a glucose monitor or how people suffering from cardiovascular disease measure their blood pressure, Augmented Mental Health technologies will become the status quo for caring for mental health.
Principles of Augmented Mental Health:
Here is a visual look into of what care will look like in the Augmented Mental Health era:
How Augmented Mental Health Will Transform Health Care
Will patients and caregivers be the only ones who’ll reap the benefits of Augmented Mental Health? Certainly, not.
Insurance providers, employers,and pharmaceutical companies will also benefit from the use of Augmented Mental Health technologies. Insurance providers will be able to offer better plans and increased access to mental health services resulting in better quality of service and increase in customer satisfaction. They will assume less risk as the insurance claims for mental health will decrease, and as disability caused by mental health issues will be reduced.
For Employers, mental health becomes a critical matter, as 1 in 3 “sick notes” from employees are for mental health-related causes. The Augmented Mental Health ecosystem, not only will help employers lower absenteeism and health care costs, but also to reduce staff turnover as employees take a more proactive role in managing their mental wellbeing leading to higher productivity and employee satisfaction.
As far as pharmaceutical companies, for the first time, objective data will be used in psychiatric drug assessments and clinical trials to measure efficacy and pave the way for the discovery of novel drug treatments for mental illness.
Finally, through such technologies, healthcare providers will be able to ensure compliance of patients to treatment and personalize this treatment to the individual based on the objective data that they will be monitoring. Also, they will be able to better manage the mental health of patients after hospitalization and in cases where mental health comes as comorbidity disorder.
This new era of Augmented Mental Health will also bring many challenges. Adoption and clinical validation of new technologies, the protection of personal data and privacy, and shaping the regulatory framework, are just some that come to mind.
All these technologies still need to get the clinical validity in order to be used for treatment purposes, and of course we have a long way to go. Although we are still a few years away from realizing Augmented Mental Health, I am confident for 3 things:
If you too believe that a change in the way we deal with Mental Health is imminent, if you believe that technology can help us make that change, then join us and help us shape the era of Augmented Mental Health.

I am the Co-founder & CEO of Sentio Solutions. The company focuses on the development of Feel, the first wristband that recognizes and tracks human emotions, to help users develop positive emotional habits and improve wellbeing.
All author postsIn the post-Covid drive for live events, ticket platforms are jumping at the opportune market time
Read more...EveryCure will leverage BioLogicAI, BioPhy’s predictive AI engine, to assess drug-disease matches
Read more...The contract will make it easier for state agencies to evaluate and implement Fusion's technology
Read more...Startup/Business
Joined Vator on
Sentio Solutions is developing digital therapeutics and biomarkers for mental health. Its premier offering, the Feel Program, is an end-to-end solution for mental healthcare that combines emotion recognition technology with real-time, AI-driven interventions, 24/7/365 personalized support, and access to therapists. The program benefits individuals who are at-risk or suffering from depression, anxiety, high stress, and burn-out through benefits sponsored by their health plan or employer.
Feel Program consists of: