This past October, telemental health platform Brightside Health, a company that delivers virtual mental health care for mild-to-severe clinical depression, anxiety, and other mood disorders, revealed that it had partnered with payers to provide care to Medicaid and Medicare members, including Optum, Blue Cross and Blue Shield of Texas, Centene, and Lucet.
This past October, telemental health platform Brightside Health, a company that delivers virtual mental health care for mild-to-severe clinical depression, anxiety, and other mood disorders, revealed that it had partnered with payers to provide care to Medicaid and Medicare members, including Optum, Blue Cross and Blue Shield of Texas, Centene, and Lucet.
Now just a few months later the company is expanding that initiative, announcing new and expanded payer partnerships to support Medicaid and Medicare on Wednesday.
That means new contracts with CareOregon to serve Medicaid and Blue Shield of California to serve Medicare Advantage and Commercial members. It also involves an expanded contract with Blue Cross and Blue Shield of Texas to include Medicare Advantage; and an expanded contract with Traditional Medicare to include Texas, California, Delaware, Arizona, New York, and Washington.
In addition, Brightside is also expanding state-by-state with Centene, including Medicaid beneficiaries with Nebraska Total Care, and with Centene’s Wellcare Medicare Advantage and AmBetter Health Exchange.
When a member joins Brightside, they start with a free assessment leading to a personalized treatment plan. From there, members can make an appointment to be seen within 48 hours and get started working with the same care team from start to finish.
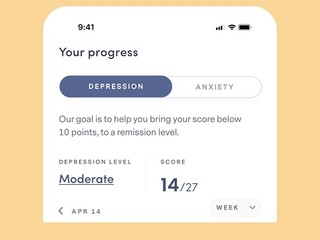
Brightside’s platform includes personalized psychiatry with PrecisionRx, which provides AI-driven recommendations based on over 100 data points, as well as real-time care management, which can track progress and identify risk levels in near-real time, allowing for automated risk escalation to the provider.
In addition, patients also get advanced quality management with ActiveSupervision, which scans charts to verify completeness and identify situations that a supervisor should review, and Crisis Care, a national telehealth program for treating individuals at elevated risk for suicide.
Serving the Medicare and Medicaid populations
While the mental health crisis continues even post-pandemic, with signs of growing depression, anxiety, suicidality, substance use, and use of the emergency department for mental health needs, that need is even greater for the Medicare and Medicaid populations, with an estimated one in four Medicare beneficiaries living with mental illness.
“Medicaid is already the largest payer from a net dollar standpoint for mental health services in the US, but only about half of people that have a mental health need in Medicaid are actually able to access care,” said Brad Kittredge, co-founder and CEO of Brightside Health.
“You’ve got a higher severity and an acuity on average in this population, a lot of people driving emergency room visits and readmissions, as well as inpatient hospitalizations. So, it’s a very acute problem with a lot of complexity and comorbidity among that Medicaid population.”
Meanwhile, on the Medicare side, there are two programs within Medicare that allow patients to access care: Medicare Part B, working directly with CMS, and Medicare Advantage. Today, about half of Medicare beneficiaries are in each program. Yet, a recent study showed that psychiatry access in Medicare Advantage networks is actually worse than in many Medicaid networks, making it increasingly difficult for seniors to be able to get the care they need.
For Brightside, once the company decided to go serve these programs, the first step was to ensure that it was aligned with all the regulatory requirements and could appropriately serve the population, Kittredge explained.
“In the case of both populations, we’ve already treated a lot of seniors and a lot of low income individuals. And so, before entering these markets, our first step was to analyze our own data, say, ‘how are we doing among those subpopulations?’ We published and peer reviewed two papers, one showing that we had a consistent impact with seniors as among our general population of patients, and the same with those individuals reporting low income,” he said.
“That gave us confidence to know that our care model can effectively engage and be impactful among these subpopulations. And that was ultimately the thing that allowed us to decide to go forward and try to meet this big market need.”
Now, with these new contracts, Brightside is serving Medicare Part B in seven states, including California and Texas, with the expectation that it will be serving all 50 states and D.C. by late summer this year, meaning 30 million additional Medicare Part B members will have access to Brightside. It’s also expecting to be able to serve the majority of Medicare Advantage members within the next 12 months as well.
On the Medicaid side, the company has partnered with Centene, the largest Medicaid payer in the US.
In terms of ROI, within 12 weeks of using Brightside, 86% of patients experience clinically significant improvement, while that number is 88% for those reporting suicidal ideation at intake. The company also sees 71% achieving remission, compared to 69% for those reporting suicidal ideation at intake. Of the patients achieving remission within 12 weeks, 65% did so within 28 days, and 82% did so within 48 days. The mean time to remission was 31 days.
For Medicare and Medicaid patients over the last few months, Brightside saw results similar to those in its broader population.
“When it comes to serving both of these populations, our priorities are very consistent with our care model overall: we want to do the hard work to really serve the hard populations and the hard cases in a way that brings real clinical rigor and measurable outcomes. We want to really raise the bar and open up opportunities to collaborate with these payer partners and, ultimately, deliver the the best possible care to patients,” Kittredge said.
“That quality bar for us is something that’s going to continue to be the focus that we’re going to raise with our technology and our data and our expert provider network.”
(Image source: brightside.com)