Value-based MSK platform Livara raises $15M
The round brings Livara's total funding to $27 million raised to date
Read more... While 156 million people, or nearly half of the country's population, got their health insurance from through their employer, only 10% of employees actually use them. That's because more than 75% of them don’t understand their health benefits or how to use them, which has consequences for both employees and employers.
While 156 million people, or nearly half of the country's population, got their health insurance from through their employer, only 10% of employees actually use them. That's because more than 75% of them don’t understand their health benefits or how to use them, which has consequences for both employees and employers.
For employees, half will delay getting care, which can lead to worse health outcomes, increases in hospital services usage, and major increases in secondary care costs. Among those who do get care, many will declare bankruptcy due to not knowing where to get cost effective care. Meanwhile, employer healthcare costs have hit a new record high every year since 1999.
Medefy Health, a mobile-first healthcare benefits navigation platform, is looking to improve this experience through real-time guidance. Earlier this week the company announced a $10 million Series A funding round led by Mercury Fund, with participation from Advantage Capital, bringing it total funding to $14 million.
"After literal millions of exchanges with members, we see the same member experience pattern emerge nearly every time. The first barrier for the member is confusion - when they need to use their health plan where do they start? What’s covered? Where can they go? How much will it cost? How do they make sense of all this confusing terminology, plan design, and benefit offerings?" Matt Scovil, the company's co-founder and CEO, told VatorNews.
The second barrier that people face is fear, meaning they know that if they make the wrong decision, choose the wrong doctor or facility, or drift out of network unknowingly, they’ll end up paying a massive deductible or out-of-pocket max cost.
And, finally, there's frustration: members want to make better decisions, but the main tools handed to them to help are archaic and unpopular, such as paper documents given to them months ago at open enrollment, their insurer’s website, and six 1-800 numbers on the back of their insurance card.
"Understanding health insurance is incredibly difficult, affording care is incredibly challenging, and trying to make better decisions with ancient tools and lack of information is nearly impossible," said Scovil.
Launched in 2018 by Scovil and Nathan Gilchrist, Medefy's chat-based platform engages health plan members through multi-channel outreach, then connects them with its team of 24/7 real human care guides and benefits experts to help schedule care with an average initial response time of under 60 seconds.
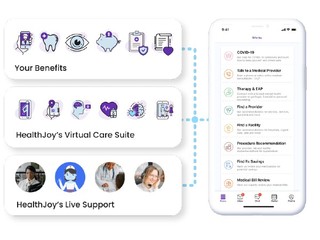
Medefy members will immediately see their entire health plan and health benefits offerings tailored to them specifically, including telemedicine and pharmacy offerings when they log into the app. If they need help, they can live-text with a real-human health benefits expert in under 60 seconds, 24/7. The company's care guides have complete access to that member’s company health plans and benefit offerings, and can answer questions, help them identify benefits they or their families can use, and can help them locate low-cost, high-quality care in minutes. The company will help them set appointments, arrange surgeries, coordinate doctors, and transfer medical records and information.
"We realized very early on that members will never be the 'informed healthcare consumers' everyone was trying to make them be," Scovil explained.
"The health insurance and benefits world is large, complex and constantly changing. But, if members could talk with someone who knew everything about their health plan in the moment of decision, they’d choose to get care at a suggested low-cost, high-quality provider 96% of the time."
The company currently serves a customer base of over 1,500 employers and their members across the U.S., including self-insured employers, insurance brokers, benefits advisors, TPAs, and enterprise groups, some of whom have seen a 3x to 5x return, with some well north of that if they’ve got more consumer-friendly health plans.
The new funding will be used to enhance Medefy's existing technology platform and artificial intelligence capabilities. That means using AI to enhance and scale its own employees as they interact with members to enhance the experience for customers.
Scovil stresses that the company sees AI as a way to enhance people, not as a replacement.
"We’ve seen big trends around either going too big, with AI-based digital health platforms that do everything, or too small, with bespoke niche digital health platforms that have very small applications also driven by AI. In the employer health space, with a couple of exceptions, both of these approaches fail," he said.
"Healthcare is a very intimate human-to-human connection, but the trend over the last eight or so years, especially in the digital health world, has been to try to replace this connection with algorithms, chat bots, and AI-generated decision trees. The average member dislikes this experience, and largely disengages with it, leaving them exactly where they started."
Going forward, the company is also looking to expand into new space, working on better, more effective and cohesive primary care experiences and smarter navigation in the Rx space.
"We started Medefy to help the average person act like an expert in healthcare. Nearly every family will interact with their health benefits or the healthcare world in the near future. While there are still people struggling with this monster alone, our mission isn’t fulfilled: to demolish barriers between healthcare and the people who need it."
(Image source: medefy.com)
The round brings Livara's total funding to $27 million raised to date
Read more...Dream Sock is an over the county monitor offering live health readings and notifications for infants
Read more...This round values the company at $2.2 billion
Read more...