When Derek from Indiana first noticed problems with his toes, he followed his doctor’s advice without question – amputation. Diabetes, they told him, was the culprit. One by one, his toes were amputated. Then half his other foot. Each procedure was presented as inevitable—a necessary sacrifice to a disease with no other options.
It wasn’t until Derek’s wife desperately called the Global PAD Association’s Leg Saver Hotline that the truth emerged. Derek had never received a proper vascular evaluation. When he finally did, doctors confirmed what we suspected—peripheral artery disease (PAD), plaque build-up in the leg arteries, was restricting blood flow to his feet. With proper intervention from a limb salvage specialist, Derek avoided further amputations.
(video below shows how Peripheral Artery Disease develops)
Derek’s case represents a disturbing trend we see daily. Every four minutes, an American undergoes a lower extremity amputation due to peripheral artery disease (PAD) and diabetes. That’s approximately 150,000 amputations annually—most of which might have been preventable with proper care, according to an NIH study. This sobering statistic represents not just a medical crisis but a failure of our healthcare system to adapt to evolving disease patterns and provide appropriate care to those most at risk.
As I’ve witnessed across America in my years advocating for PAD patients, we’re facing an unprecedented crisis in limb loss—one created by a perfect storm of evolving disease patterns, outdated treatment approaches, and perverse insurance incentives that together threaten millions of Americans with unnecessary amputations.
The “Bottoms Up” disease that’s changing everything
When vascular disease was first extensively studied decades ago, PAD typically followed a predictable pattern. Patients experienced cramping in their calves when walking (claudication), which gradually worsened until they sought medical attention. The disease primarily affected larger vessels above the knee, and treatment protocols were designed accordingly.
Today, everything has changed. PAD is increasingly presenting as a “bottoms up” disease—starting in the smallest vessels of the feet and progressing upward. These patients often don’t experience the traditional warning signs. Their first symptom might be a non-healing wound or excruciating nighttime pain.
This shift is transforming PAD into a silent epidemic. While an estimated 20 million Americans have PAD, the disease remains undiagnosed in more than half of patients until they reach advanced stages—at which point limb loss becomes a very real threat, according to a study published in the Journal of Vascular Surgery.
The clinical term for this advanced stage is critical limb ischemia (CLI) or chronic limb-threatening ischemia (CLTI), but behind this technical language lies a devastating reality: patients facing imminent amputation if blood flow isn’t restored. Research from the Society for Vascular Surgery suggests that 50-85% of these amputations might be preventable with proper diagnosis and treatment.
The severity of this condition cannot be overstated. CLI represents a major public health crisis that receives far less attention than it deserves. According to data from the CLI Global Society, CLI is responsible for more deaths over a 5-year period than any cancer except lung cancer. When comparing incident cases and mortality, CLI (58,000 deaths) surpasses colorectal cancer (49,000 deaths) and ranks as one of the leading causes of mortality among major diseases. The 5-year mortality rate for patients with CLI, according to the Global Vascular Guidelines on the Management of Critical Limb-threatening Ischemia is approximately 60%, making it deadlier than many common cancers, yet it receives a fraction of the research funding and public awareness.
The twin epidemics fueling the crisis
What’s driving this dramatic shift in how PAD presents? The answer lies in two concurrent health crises that specifically damage the smallest blood vessels first.
Diabetes, now affecting more than 37 million Americans, according to the American Diabetes Association, creates a perfect environment for small vessel damage. High blood sugar levels gradually destroy the delicate vessels in the feet and lower legs, often before patients experience any symptoms. By the time a wound appears, the underlying vascular disease may be extensive.
Chronic kidney disease represents the second epidemic contributing to this crisis, according to Centers for Disease Control and Prevention. Affecting approximately 37 million Americans, kidney disease damages small blood vessels throughout the body. When combined with diabetes—as it frequently is—the vascular damage accelerates dramatically.
The data tells a sobering story. Patients with both diabetes and kidney disease face amputation rates up to 10 times higher than the general population. Yet our healthcare system continues treating PAD as though it primarily affects larger vessels, using protocols developed decades ago.
When guidelines don’t keep pace with disease
This evolution in how PAD presents has outpaced our medical guidelines and insurance policies. Most treatment protocols were developed when PAD primarily affected larger vessels above the knee—arteries that respond well to conventional interventions like angioplasty and stenting.
The small vessels below the knee and in the foot present unique technical challenges. They’re narrower—often no wider than a coffee stirrer—more delicate, and more likely to reocclude after treatment. Successfully navigating and treating these vessels requires specialized expertise and tools.
Current PAD guidelines, while comprehensive, don’t fully address the unique challenges of this “bottoms up” disease pattern. The Global Vascular Guidelines on the Management of Chronic Limb-Threatening Ischemia provide excellent overall recommendations, but even these relatively recent guidelines don’t fully capture the changing nature of the disease. The evidence has to be generated before the guidelines can be produced, a multi-year process by the time you get all the thought leaders together to come to some consensus and then put together a published document.
The resulting gap between medical need and available limb-saving care is widening daily. As diabetes and kidney disease rates continue climbing, more patients present with small vessel disease requiring specialized interventions. However, limb-saving healthcare delivery remains constrained by a system where doctors and insurance companies must prioritize guideline-adherent care, creating barriers to the innovative approaches and clinical evidence generation needed to update those very guidelines. This self-reinforcing cycle creates an urgent need for adaptive clinical practices and accelerated research pathways that can respond to emerging patterns of disease before more preventable amputations occur.
The hidden racial and geographic disparities
This crisis doesn’t affect all Americans equally. The amputation epidemic reveals disturbing disparities along racial, geographic, and socioeconomic lines.
Multiple studies on disparaties in healthcare show black Americans face amputation rates up to four times higher than white Americans with the same disease severity. Hispanic Americans face similarly elevated risks. These disparities persist even after controlling for comorbidities and disease severity, suggesting systematic differences in care quality and access.
Geography compounds these disparities. In what researchers have termed the “amputation belt”—stretching across the southern United States from North Carolina to Texas—amputation rates are up to 500% higher than in other regions. A review of Medicare 2003 to 2006 data shows rural patients face particularly high risks, often living hours away from centers specializing in advanced limb salvage.
The anatomy of despair: why patients give up
One of the most disturbing aspects of this crisis is how it systematically breaks patients’ will to fight. The journey from initial symptoms to limb-threatening emergency often spans years, during which patients navigate a labyrinth of referrals, tests, and treatments.
By the time they reach advanced disease, many have already endured years of pain, mobility limitations, and unsuccessful treatments. When a physician then pronounces amputation “inevitable,” the psychological impact can be overwhelming.
Research on post-amputation outcomes reveals high rates of depression, anxiety, and reduced quality of life. Studies have documented depression rates as high as 41% among lower extremity amputees, with many patients experiencing significant psychological distress that persists for years after the procedure.
This psychological dynamic creates a scenario where patients consent to life-altering amputations without realizing alternatives might exist. The problem is compounded by what researchers call “therapeutic inertia”—the tendency to continue with established treatment patterns even when evidence suggests better approaches exist.
The devastating data from our frontlines
Data from our Global PAD Association’s Leg Saver Hotline confirms this systematic failure. Among more than 1,000 patients we’ve helped save from amputation, over 85% report that physicians never attempted to open their arteries before recommending limb removal, despite Society for Vascular Surgery guidelines recommending an attempt to restore blood flow prior to amputation. The majority had below-the-knee disease—precisely the “bottoms up” pattern described earlier.
Even more alarming, 35% never received any vascular evaluation whatsoever. They were simply told, like Derek from Indiana, that their amputation was “necessary due to diabetes.” Yet when these same patients finally received proper vascular assessment at our prompting, 100% were diagnosed with PAD. With appropriate intervention from limb salvage specialists, all experienced either minimized amputation or avoided it entirely.
These findings aren’t isolated to our hotline cases. Dr. Eric Secemsky’s landmark study of Medicare data confirms this pattern on a national scale. His research revealed that approximately 60% of all Medicare patients who underwent lower extremity amputations had no attempt to restore blood flow in the year prior to amputation. Even more disturbing, 90% of these patients never received a proper vascular evaluation at all—a fundamental failure to follow basic standards of care before proceeding with a life-altering amputation.
This pattern of care directly conflicts with established guidelines from both the Society for Vascular Surgery and the American Heart Association, which explicitly recommend vascular evaluation and attempts to restore blood flow before proceeding with amputation.
The way forward: recognizing the crisis
The first step toward addressing any crisis is acknowledging its existence. For too long, the amputation epidemic has remained a hidden crisis—devastating to those affected but largely invisible to policymakers and the public.
This invisibility stems partly from who the crisis affects—disproportionately older, poorer, and minority patients with multiple chronic conditions. These populations have historically had less voice in healthcare policy. Their suffering occurs largely out of public view, in rural communities and disadvantaged urban neighborhoods where healthcare access is already limited.
Breaking this silence requires understanding that amputations represent not isolated medical decisions but systematic failures across our healthcare system:
- Failure to diagnose PAD early, when interventions are most effective
- Failure to refer patients to specialists with advanced training in limb salvage
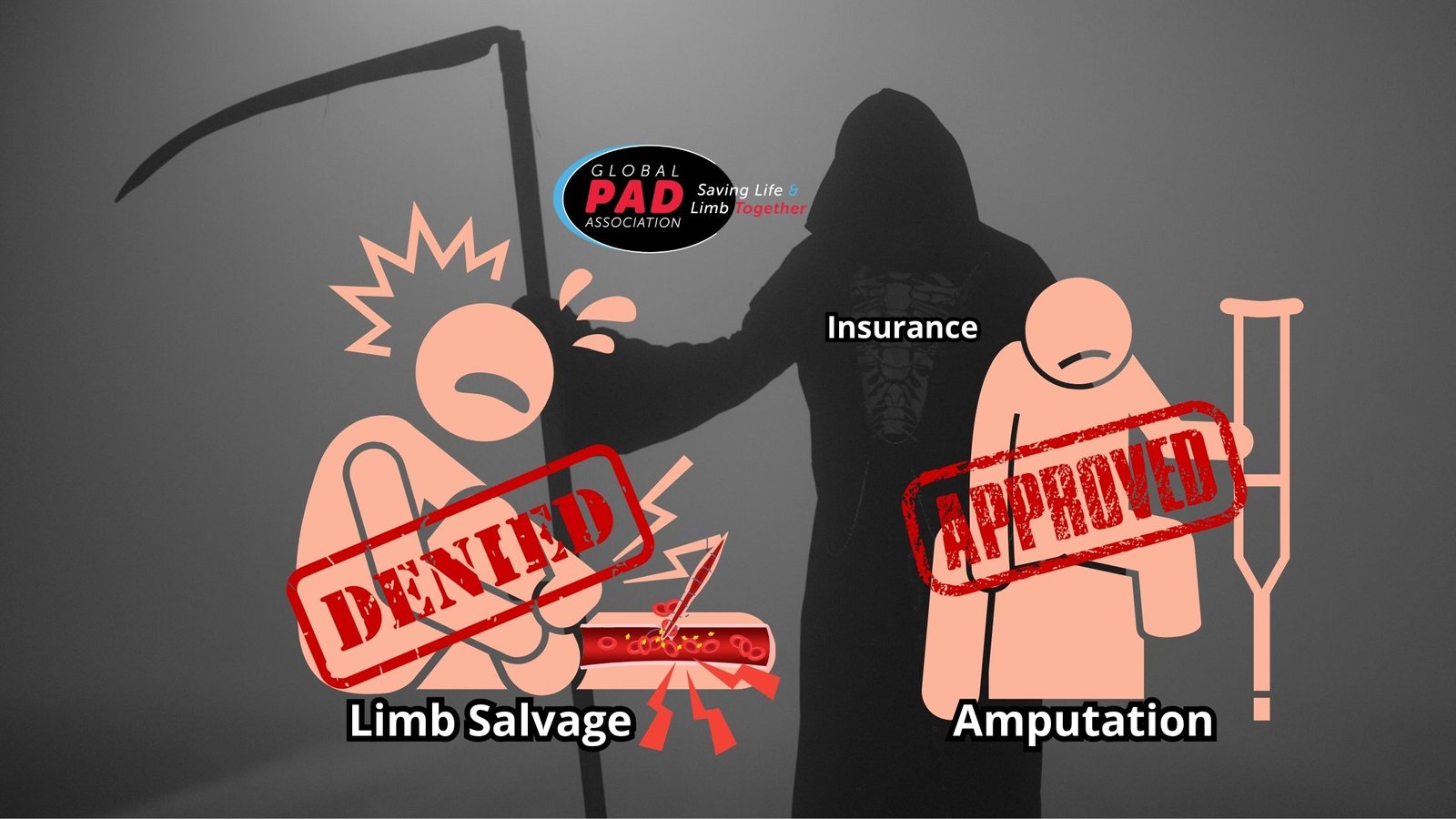
- Failure to ensure insurance covers the procedures most likely to save limbs
- Failure to address the racial and geographic disparities in amputation rates
In subsequent articles in this series, I’ll examine how insurance policies explicitly favor amputation over limb salvage, the perverse financial incentives driving these decisions, and the solutions that could dramatically reduce unnecessary amputations across America.
For now, the most important message is this: if you or a loved one faces PAD, especially if amputation has been recommended, seek a second opinion from a specialist in limb salvage. The decision you make could mean the difference between years of disability and maintaining your mobility, independence, and quality of life. If you have questions, call the Global PAD Association’s Leg Saver Hotline at 1-833-PAD-LEGS or go to PADhelp.org.
Because in America today, “nothing more we can do” too often means “nothing more we’re willing to try”—and that’s a verdict no patient should accept without question. Just ask Derek from Indiana.