Pearl Health and Wellcare team up to advance value-based care
Patients receiving care under value-based care arrangements grew by 2.3 million from 2013 to 2023
 Value-based care programs, in which clinicians incentive payments for the quality of care they provide, rather than just for performing a service, are particularly popular among Medicare plans: patients receiving care under value-based care arrangements grew by 2.3 million from 2013 to 2023, with 70% of Individual Medicare Advantage patients seeing value-based care providers in 2022.
Value-based care programs, in which clinicians incentive payments for the quality of care they provide, rather than just for performing a service, are particularly popular among Medicare plans: patients receiving care under value-based care arrangements grew by 2.3 million from 2013 to 2023, with 70% of Individual Medicare Advantage patients seeing value-based care providers in 2022.
These types of arrangements depend on getting more physicians, particularly those in primary care, on board. That's why Pearl Health, a company focused on physician enablement and risk bearing in value-based care arrangements, announced a new partnership with Wellcare, the Medicare brand of Centene, on Tuesday. The goal is to advance value-based care in collaboration with primary care physicians.
Founded in 2020, the New York-based Pearl Health's mission is enables providers to take advantage of new payment models that transition away from fee-for-service and provide compensation for keeping patients healthy, while also allowing them to proactively manage Medicare patient panels.
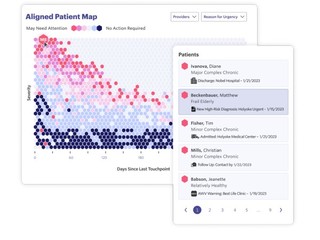
Through the Pearl Platform, providers and clinical staff can more easily identify the patients most likely to need attention across a patient panel. They can also explore detailed patient-level information with data across providers and facilities, such as hospital admissions, new diagnoses, and new medications.
For example, the Pearl Platform gives providers and clinical staff admit, discharge, and transfer alerts, so they have the information they need to effectively coordinate care following acute or post-acute events and prevent costly, avoidable hospital readmissions. The company also provides turnkey reporting, giving primary care organizations visibility into the most important determinants of success in value-based models so they can identify where they could deliver better care at a lower cost.
Wellcare, meanwhile, offers Medicare products such as Medicare Advantage and Medicare Prescription Drug Plans (PDP). The company offers healthcare access to more than 1.2 million Medicare Advantage members and 4.1 million PDP members across all 50 states.
The collaboration between Pearl and Wellcare, which involves a multi-year Medicare Advantage partnership establishes a pathway to sharing increased financial risk, will allow the two companies to accelerate their collaboration on several initiatives, including value-based care models, as a way to improve health outcomes and better control costs for Wellcare Medicare Advantage members.
Pearl Health offers primary care providers participating in Wellcare's networks access to data insights, financial tools, practice enablement technology, and value-based care services.
Currently, this program is live in South Carolina, and the two companies are planning on expanding it nationwide.
"This partnership enables Pearl to expand its technology and capabilities across both Traditional Medicare and Medicare Advantage plans," Michael Kopko, CEO & co-founder of Pearl Health, said in a statement.
"With Wellcare's partnership, physicians will now be able to manage their patient panel — focusing on improving quality and lowering costs — more efficiently across a growing portion of their Medicare population."
In the past year Pearl Health also partnered with Story Health to provide continuous cardiovascular care, as well as with Walgreens to put more tools and resources into the hands of primary care physicians.
(Image source: pearlhealth.com)
Related News
Pearl Health raises $75M to help PCPs transition to value-based care


