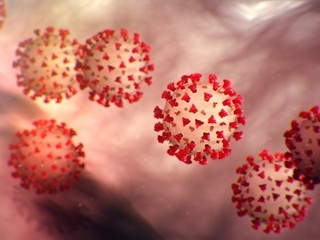
Will coronavirus lead to open borders for healthcare?
Optum, Ginger, BetterHelp, Khosla Ventures debated the topic at Invent Health's first virtual salon

One of the big unknowns right now is what the American healthcare system will look like when the coronavirus crisis finally ends. There's no doubt it will be different in some ways, and hopefully some lessons will be learned to make it work better for both patients and providers, but what that means will only become clear in the months and years ahead.
For example, will we see a change in regulation allowing doctors to treat patients across state lines? The Trump administration announced last week that the Department of Health and Human Services issued a regulation that would "allow all doctors and medical professionals to practice across state lines to meet the needs of hospitals that may arise in adjoining areas," though it's still not clear what exactly that means, and what that regulation would look like.
Regulations, after all are complicated, so it seems unlikely this would be anything more than a temporary order. It's also not exactly clear what the states will have to say about it.
All of these topic were broached at the virtual healthcare salon held by Vator, along with HP and USCF Health Hub, last week, in a panel moderated by Dr. Archana Dubey (Global Medical Director, HP Health Centers, HP), and Bambi Francisco Roizen (Founder and CEO, Vator). The speakers were Alex Morgan (Investor, Khosla Ventures), Russell Glass (CEO, Ginger.io), Tim Blevins (SVP Behavioral Health, UnitedHealthCare Optum) and Alon Matas (President, Teladoc’s BetterHelp).
Dubey asked the panel to discuss rules and regulations they are seeing change right now.
"Are you starting to see that you’re expanding your virtual care or your sessions or text ability across state borders?" she asked, to which Blevins responded that, "It’s a little too early to know" what exactly this would look like but that "we were actually already seeing a lot of psychiatrists, in particular, who were doing a lot of work virtually, get licensed in other states."
While there's a lot of cost and paperwork involved with getting licensed in a different state, Blevins noted, he still thinks it's something more mental health workers will wind up doing going forward.
Glass brought up that Ginger was already structured to operate in all 50 states, and that its therapists have, on average, seven state licenses, so this is something it has already been doing anyway. The company actually takes care of relicensing for its therapists, something that Glass also noted is expensive which "takes resources away from actually providing care, and actually delivering the value that we want to deliver to customers."
Getting rid of the cost and the time to get licensed and relicensed will be a win for everybody involved, he said.
"The easier this gets over time, and the reduction of resources that we need to put towards these state licensing requirements, it’s a win not only for us but for the people we’re caring for. We’ll manage the quality, and let’s get rid of the regulations so we can deliver great quality across all state lines."
While Glass and Blevins were optimistic that these changes to licensing and regulations will happen, BetterHelp's Mata took the "more pessimistic approach," noting that it's unlikely that anything will actually happen.
"There’s a big gap between the walk and the talk. The President says, ‘It’s an emergency, we have to open up,’ in reality almost nothing happens. That’s the situation right now. If you’re a licensed therapist in Nevada, at this point you cannot provide services in California. You just cannot. If you go and try to transition your license from Nevada to California, it will be somewhere between six months to two years. Nobody’s going to do that," he said, noting that people bring this idea up every time there's a crisis and it never actually happens thanks to opposition from local boards.
"Every time there is a big declaration of, ‘Yes, we know we need to figure this out. It doesn't make sense, we need more mental healthcare, not just in these kind of times but there’s a shortage all the time and this can definitely be almost a magical solution,’ but when it trickles down to the state boards, to the MFT boards, to the LPC boards, to the social workers board, to the psychologists board, somehow it gets stuck."
The reality is, he said, that "even when we’re in the middle of this emergency and crisis, if a therapist is not licensed in the state of the client they cannot provide services to that client."
Khosla Venture's Morgan countered by bringing up numerous examples of how things have changed thanks to moments of crisis over the years, calling coronavirus "a once-in-a century situation."
"We likely will emerge from this with a number of improvements in our healthcare system, and in our world in general. It may be very hard to reintroduce these barriers once people have seen what is actually possible, whether that’s a relaxation of a lot of requirements through channel or traction, waiving HIPAA requirements so people can access different channels. In general, we will move towards a situation with much more increased fluidity in the care delivery model, because it will be hard to step back," he said.
He compared it to the changes in the ride-sharing industry over the last decade, where consumer demand forced an entrenched and monopolistic industry, in this case the taxi services, to change their model because that's what consumers wanted.
"The fact that the majority of the public find the ease of access to those services was so incredibly powerful and so useful that it has basically preempted special interest groups and barriers to their operation have gone down," he said.
More pointedly, he compared what's happening now to the HIV/AIDS crisis of the 1980s, and the changes that brought in terms of how doctors deliver care.
"If you look at standards of care or practices of care in blood-borne pathogens prior to AIDS and HIV, providers in trauma cases often did not wear gloves. People would do all kinds of care maneuvers that now would be unthinkable. HIV and AIDs transmission is thankfully less of a concern than it was, although it’s still a concern, but all of medicine have instituted much better procedures and we’re never going to walk back from that."
Matas responded that there are 200 regulatory bodies around mental health, meaning about four in every state, and that not a single one of them have actually made any of these changes so far that would allow therapists from other states to work with people in their state.
"They all have that power, they could have all done this, and none of the 200 has done this, and we’re a month in," he said.
Morgan then gave another example of how a crisis forced a change: 9/11 brought about the Transportation Security Administration, which now has an $8 billion annual budget.
"We can argue about whether that’s a net positive or a net negative on society, but there was a huge shift way in the way that people travel as an outcome of a disaster and an event that promoted change. So, I think significant change is possible and likely to happen," he said.
"Unlike some of the regulations around travel, where people can debate how valuable it is, certainly improving access to care and reducing barriers will be something that has a social positive benefit, as well basically lifestyle and care procedures that reduce virus transmission will clearly a net positive economic and social benefit."
If someone is sick, said Morgan, "and we create lower barriers for you getting care in your home and not going to a provider, not getting other people sick in the waiting room, those are social and care delivery changes that will come and they will be a net long-term benefit for everyone."
Glass spoke up again and mediated, telling Morgan and Matas that they were both correct in how they are viewing this.
"It’s going to take longer than you think, and it’s going to happen, but it’s a morass right now. The state compacts that have come together are wildly helpful, so there is precedent for some of this and the 15 or 17 states that have come together and said, ‘We’re going to follow the same rules, and we’re going to use the same licensure,’ there’s a model for this if the rest of the states can get on board," he said.
Thanks to our sponsors: UCSF Health Hub, HP, Betterhelp, Avison Young, Advsr, Scrubbed, and Stratpoint.
(Image source: findwell.com)
Related Companies, Investors, and Entrepreneurs
BetterHelp
Startup/Business
Joined Vator on
BetterHelp changes the way people get help to conquer life's challenges.
Facing obstacles alone can be daunting. Support and guidance from a professional counselor has been shown to make big changes. We created BetterHelp so anyone can have convenient, discreet, and affordable access to professional help.

Khosla Ventures
Angel group/VC
Joined Vator on
Khosla Ventures offers venture assistance, strategic advice and capital to entrepreneurs. The firm helps entrepreneurs extend the potential of their ideas in both traditional venture areas like the Internet, computing, mobile, and silicon technology arenas but also supports breakthrough scientific work in clean technology areas such as bio-refineries for energy and bioplastics, solar, battery and other environmentally friendly technologies. Vinod was formerly a General Partner at Kleiner Perkins and founder of Sun Microsystems. Vinod has been labeled the #1 VC by Forbes and Fortune recently labeled him as one the nation's most influential ethanol advocates, noting "there are venture capitalists, and there's Vinod Khosla." Vinod Khosla founded the firm in 2004.

Bambi Francisco Roizen
Joined Vator on
Founder and CEO of Vator, a media and research firm for entrepreneurs and investors; Managing Director of Vator Health Fund; Co-Founder of Invent Health; Author and award-winning journalist.
Archana Dubey, MD
Joined Vator on
Global Medical Director, Hewlett-Packard Enterprises
Alon Matas
Joined Vator on
I build, fix and break things online.
Russell Glass
Joined Vator on
Related News


Meet Tim Blevins, SVP Behavioral Health, UnitedHealth Group Optum

Coronavirus will change healthcare as we know it